Cognitive Behavioral Therapy for Insomnia (CBT-I)
Based on over 35 years of research and clinical experience, CBT-I is the recommended first line treatment for insomnia disorder, that is chronic insomnia that persist over at least 1 month. CBT-I addresses the root causes of what makes someone transition from the occasional bad nights to chronic insomnia by getting the person to:
Learn about how sleep systems works
Break down sleep-related habits and thought patterns that maintain insomnia over time
Implement guided progressive and personalized adjustments of the sleep schedule that rebalances homeostatic sleep pressure and stabilizes the circadian clock to naturally strengthen the sleep system
Cognition
Behaviours
Therapy
Helps recognize and change unhelpful thoughts about sleep—like worrying about not sleeping—which can fuel anxiety and make insomnia worse
Tailored changes in sleep schedules and sleep-related behaviors to boost natural sleepiness
Provides long-lasting skills to address the root causes of chronic insomnia by strengthening the body’s natural sleep system
With durable benefits that typically outlast those of pharmacological treatments (Moring et al, …), It is effective across age groups and clinical populations. For instance, in people who also have different types of mental disorders (from depression to post-traumatic stress disorder), it not only improves sleep, but mental health symptoms (Hertenstein et al, 2022, Sleep Medicine Review -> https://www.sciencedirect.com/science/article/pii/S1087079222000107).
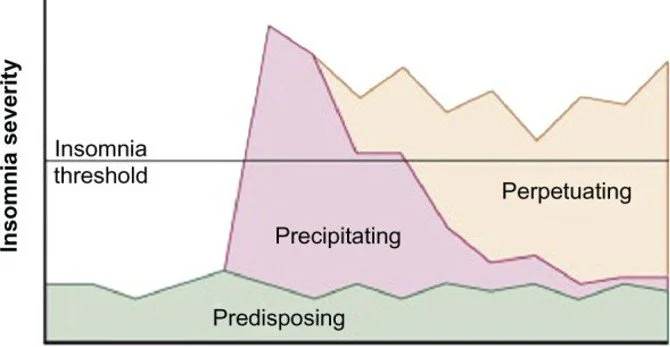
Conceptual Model
CBT-I is grounded in the “3P” model of insomnia (predisposing, precipitating, perpetuating factors). While acute insomnia may be triggered by stressors or illness, chronic insomnia is maintained by maladaptive sleep habits, conditioned arousal, and unhelpful beliefs about sleep. CBT-I targets these perpetuating factors to restore healthy sleep regulation.
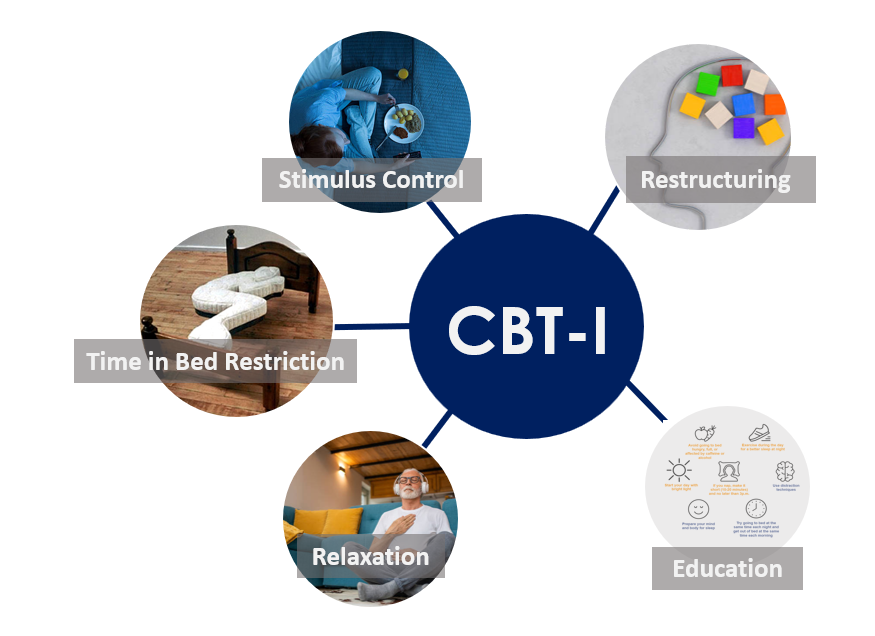
Core Components
CBT-I is a multicomponent intervention, usually delivered over 4–8 sessions.
Key elements include:
Sleep Education: Patients receive education about normal sleep physiology, circadian rhythms, and sleep need variability. Healthy sleep practices are often discussed, but this alone is insufficient to treat chronic insomnia.
Stimulus Control: This component targets conditioned arousal and aims to re-associate the bed and bedroom with sleep rather than wakefulness and negative feelings like frustration and performance anxiety linked to sleep. The patient is carefully walked through the rationale for : going to bed only when sleepy; using the bed only for sleep and sex; leaving the bed if unable to sleep; rising at a consistent time; and avoiding daytime napping.
Time in Bed Restriction: This component consolidates sleep by limiting time in bed to the actual sleep time, thereby increasing homeostatic sleep pressure. Time in bed is gradually expanded every 1-2 weeks as sleep efficiency and sleepiness improve. Although counterintuitive and initially associated with increased daytime sleepiness, this is a critical CBT-I component. Just like stimulus control, it often benefits from ongoing support and personalized troubleshooting.
Cognitive Therapy: Cognitive restructuring focuses on address dysfunctional beliefs and catastrophic thinking about sleep (e.g., “If I don’t sleep 8 hours, I won’t function tomorrow”). Patients learn to identify and challenge unhelpful thoughts, reduce performance anxiety around sleep, and adopt more flexible expectations.
Relaxation: Methods such as progressive muscle relaxation, diaphragmatic breathing, or mindfulness can be used to attenuate somatic and cognitive arousal that interferes with sleep initiation and maintenance.
Efficacy and Indications
CBT-I notably produces moderate to large improvements in sleep onset latency, wake after sleep onset and sleep efficiency. Benefits are sustained for months to years post-treatment, since it also equips patients to anticipate and deal with relapses. It is effective even when insomnia co-exists with other conditions like depression, anxiety, chronic pain, cardiovascular disease, cancer, and even other sleep disorders like sleep apnea (although comorbid sleep disorders should also be actively treated). CBT-I can also facilitate tapering of hypnotic medications and reduce long-term sedative use.
Delivery Formats
CBT-I can be delivered individually or in groups, in person or via telehealth. Bibliotherapy and Digital CBT-I programs have demonstrated efficacy and can increase access where trained providers are limited. See available resources in the section below.
Safety and Contraindications
CBT-I is generally safe. Caution is warranted with time in bed restriction in patients with epilepsy, bipolar disorder, untreated sleep apnea, or high fall risk. Screening for other sleep disorders (e.g., sleep apnea, restless legs syndrome) and significant psychiatric conditions is recommended prior to initiation.
Clinical Integration
Healthcare providers play a key role in identifying insomnia, providing brief education, and referring patients to CBT-I specialists and resources. Given its strong evidence base and favorable risk–benefit profile, CBT-I should be prioritized for the treatment of chronic insomnia.
Available CBT-I Resources
Self-Help Tools
Books
Evidence-based digital self-help tools and websites
Doze - For youth
Bilingual Free Online CBT-I (COMING SOON)
Since CBT-I is often offered by trained psychologists, you can also contact your province's psychologists college. Click HERE to access the list of Provincial and Territorial regulatory bodies.